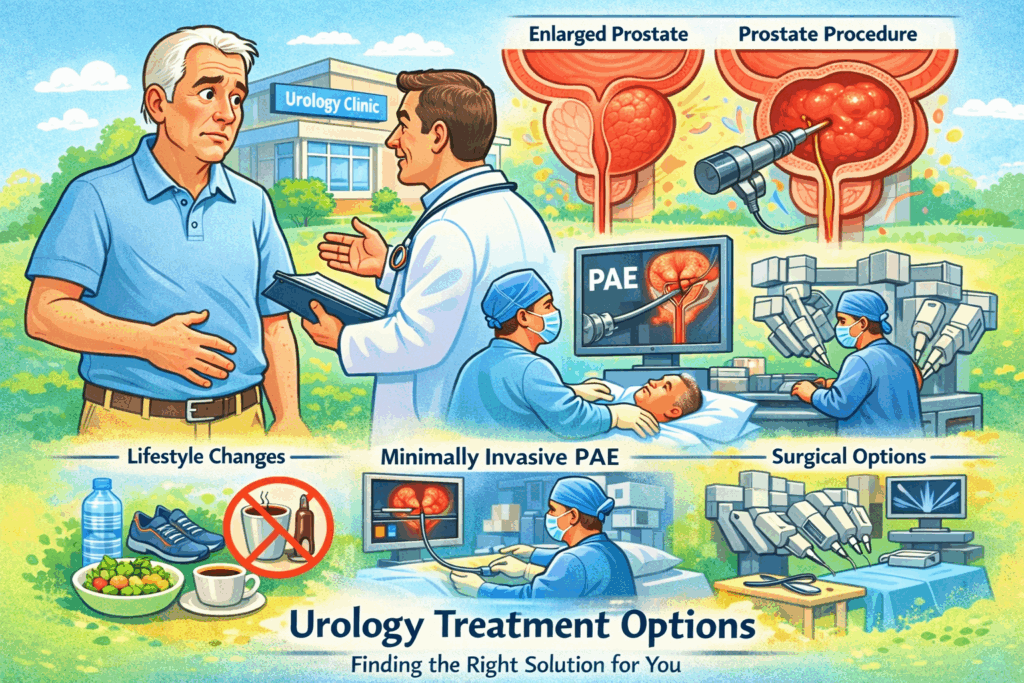
When you’re dealing with urinary problems or prostate issues, finding the right urology treatment options can feel overwhelming. You want answers that make sense for your body and your life. This guide walks you through what’s available so you can have better conversations with your doctor.
Modern medicine offers more choices than ever before. From simple lifestyle changes to advanced surgical procedures, there is a wide spectrum of solutions. The challenge is figuring out which approach best fits your specific situation.
Understanding Your Urology Treatment Options
Most urological conditions don’t have just one solution. Doctors typically start with the least invasive option and work up from there. This approach prioritizes safety while still addressing symptoms effectively.
Common conditions such as benign prostatic hyperplasia (BPH) involve the prostate gland. As men age, the prostate naturally continues to grow. Over time, this enlargement can compress the urethra and interfere with normal urinary flow.
Your symptoms, age, and overall health all play a role in determining the best path forward. What works for one person may not be right for another. Prostate treatment plans must be personalized for the best outcomes.
Lifestyle Changes That Make a Difference
Before jumping to medications or procedures, simple adjustments may ease mild to moderate symptoms. Consulting your primary care doctor is a great first step. Cutting back on caffeine and alcohol can reduce bladder irritation and urgency.
These drinks increase urine production and can worsen frequency. Regular physical activity also helps. Exercise supports overall urinary health and may reduce inflammation.
Kegel exercises strengthen pelvic floor muscles, improving bladder control. Small changes add up over time. Timing your fluid intake so you drink less before bed can also mean fewer nighttime bathroom trips.
Prostate Artery Embolization as an Alternative
Prostate artery embolization (PAE) is a minimally invasive option that doesn’t involve cutting. An interventional radiologist threads a catheter through blood vessels in the groin to reach the prostate artery and blocks blood flow to shrink the gland.
This approach works well for men who aren’t good surgical candidates or who’ve already had other procedures. It serves as a viable enlarged prostate treatment for those who cannot undergo traditional surgery.
PAE can also be combined with other treatments for larger prostates. Recovery tends to be easier than with standard surgery, and many patients experience relief without a significant risk of sexual side effects.
Surgical Solutions for Serious Cases
Sometimes surgery becomes necessary when other treatment options haven’t worked. Transurethral resection of the prostate (TURP) remains a gold standard. A scope removes excess tissue from inside the prostate to open the urinary tract.
Holmium laser enucleation of the prostate (HoLEP) is especially effective for larger prostates. The holmium laser removes large amounts of obstructive tissue and allows for laboratory analysis of what’s removed. It’s highly effective but requires specialized training.
Robotic-assisted prostatectomy may be used for very large prostates or certain cancer cases. The precision of robotic instruments allows surgeons to operate in tight spaces. For benign conditions, removing obstructive tissue is the main goal. Hospital stays are usually short even for these larger procedures.
How Doctors Choose the Right Approach
Your urologist considers multiple factors when recommending treatment. Gland size is a major one. Some therapies work better for smaller prostates, while others are more effective for larger glands.
Symptom severity and how much symptoms interfere with daily life also matter. A history of urinary tract infections or bladder issues can influence the choice. Your overall health and other medical conditions are important too, since heart or lung disease may limit surgical options.
Age also plays a role. Younger men may prioritize preserving sexual function, while older men may focus more on durability and symptom relief.
What to Expect During Recovery
Recovery varies depending on which treatment you choose. With medications, there’s usually no downtime. Minimally invasive procedures may have you back to normal activities within one to two weeks.
Traditional surgeries require more recovery time. You may have a catheter for a few days to help drain the bladder. Most men experience temporary urinary leakage that improves over weeks to months.
Following your doctor’s instructions makes a big difference in outcomes. Taking it easy helps prevent complications such as infection. Pelvic floor physical therapy can also speed recovery.
Comparing Your Options
Weighing the pros and cons of different treatments helps you make an informed decision.
- Medications: No downtime, moderate effectiveness, possible dizziness or retrograde ejaculation
- Rezūm Therapy: 1–2 weeks recovery, high effectiveness, temporary urinary symptoms
- GreenLight Laser: 1–2 weeks recovery, very high effectiveness, bleeding or infection
- TURP Surgery: 2–4 weeks recovery, very high effectiveness, incontinence or sexual side effects
No treatment is perfect for everyone. Some men value quick recovery, while others want the most definitive long-term solution.
Questions to Ask Your Urologist
Coming to your appointment prepared helps you get better answers. Ask about success rates for each option given your anatomy. Find out what recovery really looks like day by day.
Understanding potential complications matters just as much as knowing benefits. Ask whether symptoms commonly return later. Don’t hesitate to ask about your doctor’s experience with each technique.
The Role of Diet, Supplements, and Weight
Dietary changes may support urinary health, though they aren’t a substitute for medical care. Saw palmetto and beta-sitosterol are popular supplements, and some studies suggest moderate symptom improvement.
Reducing red meat and increasing vegetables appears beneficial for prostate health. Tomatoes contain lycopene, and green tea offers antioxidants that may reduce inflammation.
Obesity can worsen urinary symptoms and complicate surgery. Losing excess weight often improves symptoms and lowers the risk of bladder problems. Even modest weight loss can make a noticeable difference.
Conclusion
Managing urology treatment options doesn’t have to be confusing or frightening. From lifestyle changes and medications to minimally invasive procedures and surgery, you have choices.
Every man’s situation is different, so what works for someone else may not be your best option. Understanding the benefits and risks of each approach helps you make confident decisions.
Treating urological issues is about improving quality of life. Whether you need medication or a procedure to remove prostate tissue, relief is possible. With the right plan, most men see meaningful improvement in their symptoms.